To Buy Azithromycin Online Visit Our Pharmacy ↓

Overview of Azithromycin: Usage and Mechanism
Azithromycin is a widely used antibiotic belonging to the macrolide class, primarily indicated for infections like respiratory tract infections, skin infections, and sexually transmitted diseases. It functions by binding to the 50S ribosomal subunit of susceptible bacteria, inhibiting protein synthesis, and thereby exerting a bacteriostatic effect. This mechanism ensures a broad spectrum of activity against both Gram-positive and Gram-negative bacteria.
Its unique pharmacokinetic properties, such as extensive tissue penetration and prolonged half-life, allow for short and convenient dosing regimens, often making it a first-line choice for various infections. Despite its efficacy, the overuse and misuse of azithromycin have raised significant concerns regarding antibiotic resistance.
| Usage | Mechanism |
|---|---|
| Respiratory infections, skin infections, STDs | Binding to 50S ribosomal subunit, inhibiting protein synthesis |
| Convenient dosing regiments due to long half-life | Bacteriostatic effect |
Emerging Concerns: Antibiotic Resistance Development

Azithromycin, a member of the macrolide antibiotics class, plays a crucial role in treating various bacterial infections. However, its widespread utilization has sparked significant concerns regarding the acceleration of antibiotic resistance. Bacterial strains exposed repeatedly to azithromycin can develop resistance mechanisms, rendering the antibiotic less effective over time. This resistance compromises the drug's ability to combat common infections like respiratory illnesses and sexually transmitted infections.
Research highlights a growing trend of azithromycin-resistant bacteria worldwide. Such resistance can lead to prolonged illness durations, increased medical costs, and a higher likelihood of complications. Public health officials emphasize the importance of prudent azithromycin use to preserve its effectiveness for future generations.
Epidemiological Data: Global Impact Analysis
Azithromycin’s broad-spectrum efficacy has led to its widespread use globally, but this has not come without repercussions. Various epidemiological studies highlight an alarming rise in resistant bacterial strains, particularly in regions with high azithromycin consumption. In some countries, resistance rates have surged to concerning levels, posing significant public health challenges.
The global impact analysis reveals stark disparities across different regions. For example, Southeast Asia reports higher resistance proportions compared to Europe or North America. This variation underscores the importance of region-specific policies to manage antibiotic use and mitigate resistance development.
Increasing resistance is not just a statistical concern but translates into real-world medical challenges. Hospital reports indicate longer stays and more complicated treatment regimens for infections once easily treated with azithromycin. This necessitates urgent action to both understand the epidemiological trends and implement effective antimicrobial stewardship worldwide.
Molecular Mechanisms of Resistance to Azithromycin

Bacteria develop resistance to azithromycin through a variety of mechanisms. Some bacteria gain the ability to efflux the antibiotic out of their cells, reducing its intracellular concentration and effectiveness. Others undergo genetic mutations in ribosomal RNA or ribosomal proteins, changing the antibiotic's binding site and rendering it ineffective. Horizontal gene transfer also plays a crucial role, where resistance genes are shared between bacterial populations via plasmids. Methylation of ribosomal RNA is another common resistance mechanism, which prevents azithromycin from binding to its target. These molecular changes pose significant challenges for treating infections and highlight the urgent need for new therapeutic strategies.
Clinical Implications: Treatment Challenges and Failures
Azithromycin has long been a go-to antibiotic for treating a range of bacterial infections, from respiratory tract infections to sexually transmitted diseases. However, its widespread use is now proving to be a double-edged sword. Clinicians are increasingly encountering cases where azithromycin is losing its effectiveness. In particular, treatment failures are becoming alarmingly common, signaling the rise of resistant bacterial strains.
For instance, studies have reported significant treatment failures in conditions like chlamydia and gonorrhea, where azithromycin was once highly effective. These resistant infections not only complicate treatment protocols but also impose greater healthcare costs and extend recovery times. Unfortunately, such challenges necessitate the frequent revision of clinical guidelines, often leaving healthcare providers scrambling to adapt.
| Condition | Effectiveness of Azithromycin |
|---|---|
| Respiratory Infections | Decreasing due to resistant strains |
| Chlamydia | Increased treatment failures |
| Gonorrhea | Significant resistance observed |
The uphill battle against resistant strains means that alternative antibiotics often have to be employed, sometimes with less optimal safety profiles. Thus, the medical community faces the compelling need to innovate and identify new treatment strategies to mitigate these challenges.
Strategies to Mitigate Resistance: Policy and Practice
To combat the rising threat of azithromycin-resistant bacteria, a multifaceted approach is crucial. In policy, stricter regulations on antibiotic prescriptions and the promotion of stewardship programs can curb overuse. Healthcare providers should adhere to guidelines mandating the use of azithromycin only when necessary and encourage routine surveillance for resistance patterns.
On the practice side, there must be an emphasis on improving diagnostic accuracy to ensure appropriate antibiotic selection. Additionally, educating patients about the importance of completing prescribed antibiotic courses can prevent the survival and proliferation of resistant strains. Combining these strategies, both policy-driven and practice-oriented, can significantly mitigate the development of resistance to azithromycin.
Customer Service
Call us (702) 476-6762 or (858) 643-5555
Email address: awells@phamatech.com
About Phamatech, Inc.
Founded in 1991 by a small group of dedicated scientists and business executives, Phamatech Laboratory & Diagnostics, Inc. is a manufacturer and global provider of diagnostic products with focus on Infection, Toxicology, and Disease. Staring in 2020 Phamatech Inc. offers COVID-19 testing services in San Diego, CA; Las Vegas, NV; Palm Beach, FL and Los Angeles, CA.
Phamatech’s mission and values of quality, assurance, accountability, dependability and reliability has revolutionized its growth to become a global success with its on-site test products and a state-of-the-art testing facility. Technology and innovation in drug and genetic testing is the driving force helping Phamatech develop new technologies to better human lives. Here at Phamatech, Health and Lives matters to us! Your health is our priority.
PHAMATECH Las Vegas in the Media
COVID testing clinics report high volume of patients ahead of the new year
Angel Spears an operations coordinator for Phamatech said she expects more people to get tested after the new year’s eve weekend. “We’ve been quite busy, our system has been pretty efficient, fast in and out,” said Spears. Our turnaround time for our PCR test is 24 to 30 hours give or take and our rapid antigen is about 15 to 30 minutes.”
Las Vegas lab explains how it gets COVID-19 test results
"We went from about 40 to 70 people to ... 200 to 300 people a day," said Angela Spears, operations manager at Phamatech Labs in Las Vegas.
Our Laboratory
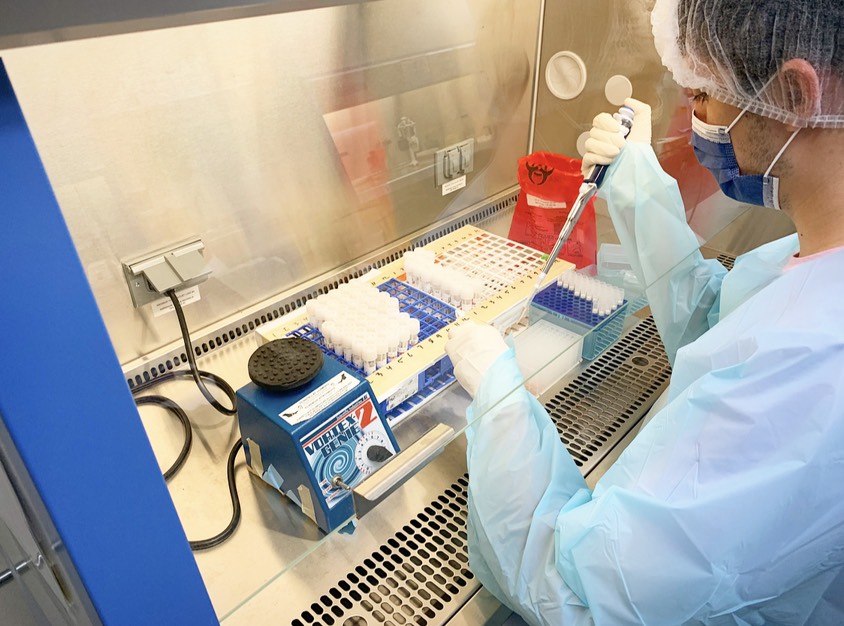


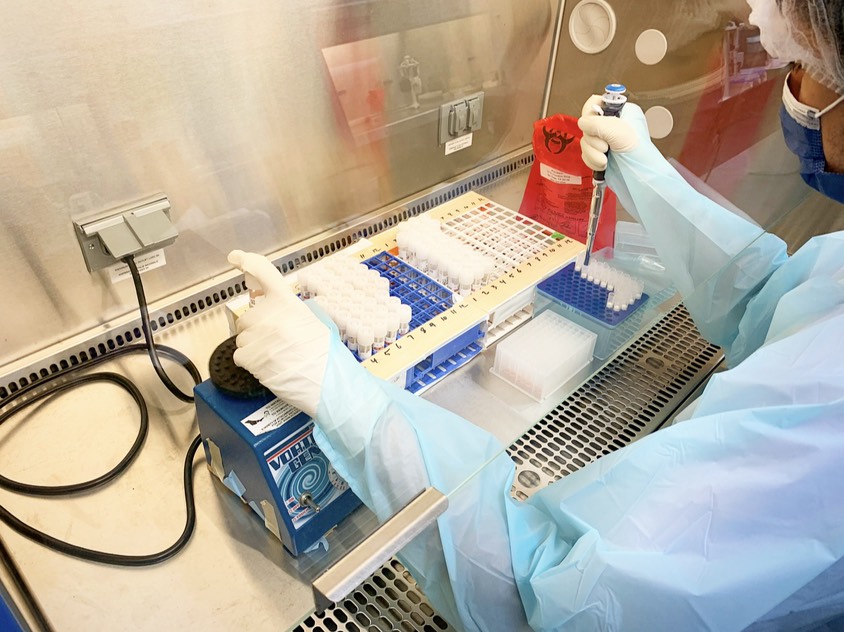
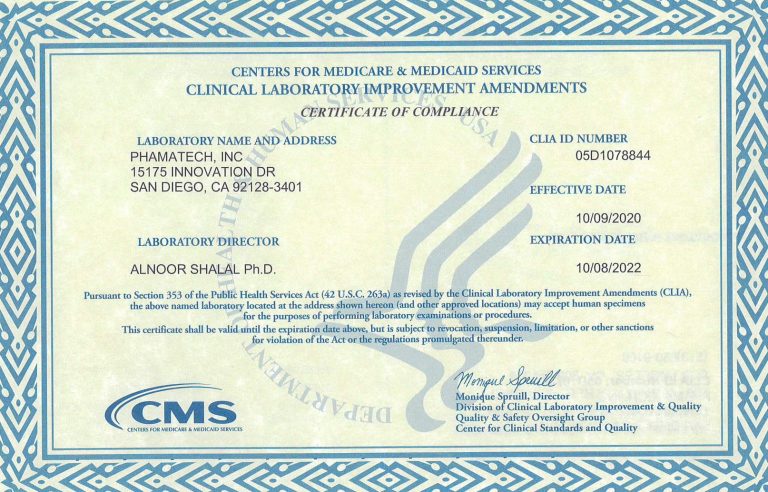
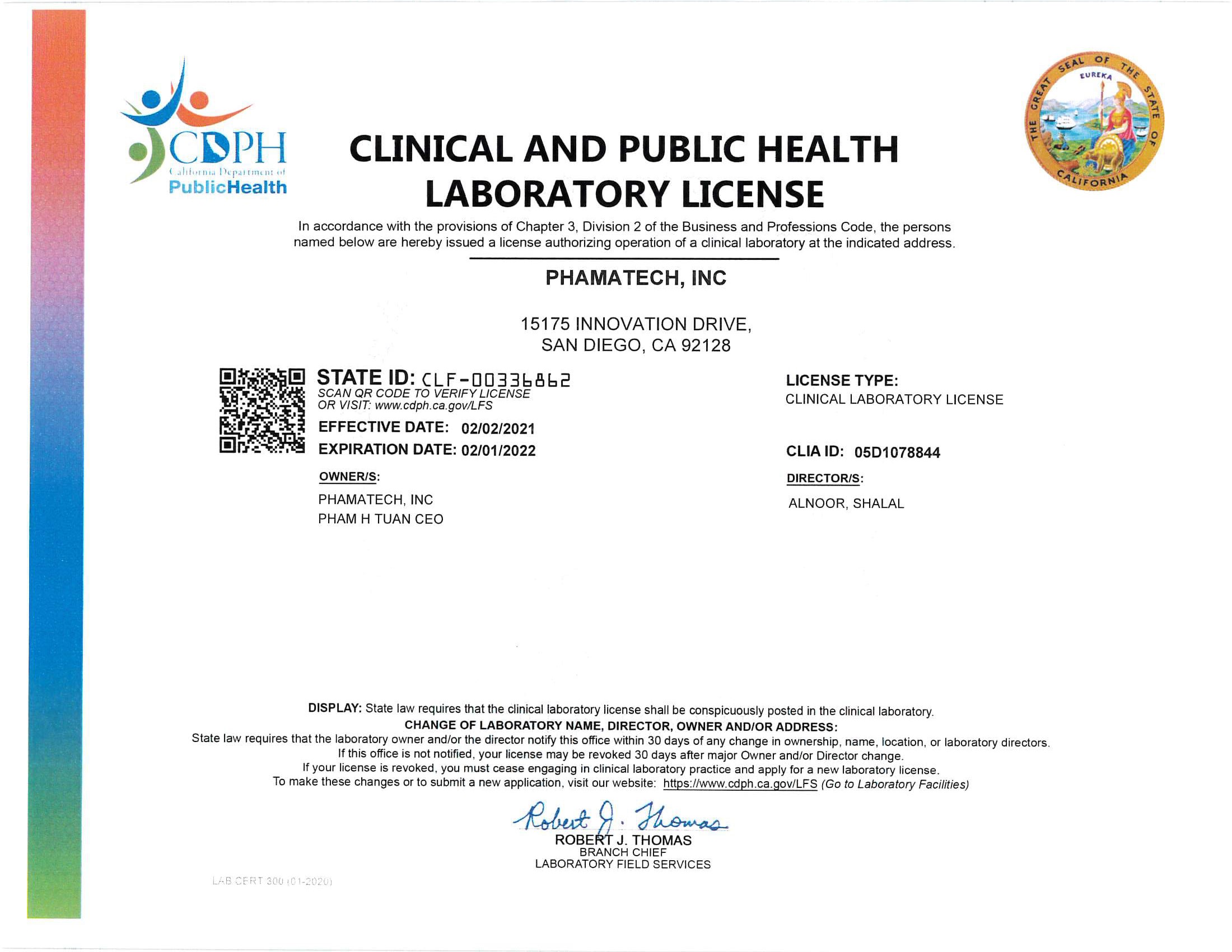
Laboratory Licenses and Certificates
.